Intensive Care Unit, Affiliated Hospital of Medical College, Qingdao University, Qingdao 266003, China
Corresponding Author:Bang-xu Yu, Email: yubangxu@126.com
Effects of early rehabilitation therapy on patients with mechanical ventilation
Ze-hua Dong, Bang-xu Yu, Yun-bo Sun, Wei Fang, Lei Li
Intensive Care Unit, Affiliated Hospital of Medical College, Qingdao University, Qingdao 266003, China
Corresponding Author:Bang-xu Yu, Email: yubangxu@126.com
BACKGROUND:For patients in intensive care unit (ICU), mechanical ventilation is an effective treatment to survive from acute illness and improve survival rates. However, long periods of bed rest and restricted physical activity can result in side effects. This study aimed to investigate the feasibility of early rehabilitation therapy in patients with mechanical ventilation.
METHODS:A randomized controlled trial was carried out. Sixty patients, with tracheal intubation or tracheostomy more than 48 hours and less than 72 hours, were admitted to the ICU of the Affiliated Hospital of Medical College, Qingdao University, from May 2010 to May 2012. These patients were randomly divided into a rehabilitation group and a control group. In the rehabilitation group, rehabilitation therapy was performed twice daily, and the training time and intensity were adjusted according to the condition of the patients. Early rehabilitation therapy included heading up actively, transferring from the supine position to sitting position, sitting at the edge of the bed, sitting in chair, transferring from sitting to standing, and ambulating bedside. The patient's body mass index, days tofirst out of bed, duration of mechanical ventilation, length of ICU stay, APACHE II score, highest FiO2, lowest PaO2/FiO2and hospital mortality of patients were all compared between the rehabilitation group and the control group. The differences between the two groups were compared using Student's t test.
RESULTS:There was no significant difference in body mass index, APACHE II score, highest FiO2, lowest PaO2/FiO2and hospital mortality between the rehabilitation group and the control group (P>0.05). Patients in the rehabilitation group had shorter days tofirst out of bed (3.8±1.2 d vs. 7.3±2.8 d; P=0.00), duration of mechanical ventilation (5.6±2.1 d vs. 12.7±4.1 d; P=0.005) and length of ICU stay (12.7±4.1 d vs. 15.2±4.5 d; P=0.01) compared with the control group.
CONCLUSION:Early rehabilitation therapy was feasible and effective in improving the outcomes of patients with mechanical ventilation.
Early rehabilitation therapy; Mechanical ventilation; Intensive care unit; Hospital mortality; APACHE II score
INTRODUCTION
For patients in intensive care unit (ICU), mechanical ventilation is an effective treatment to survive from acute illness and improve survival rates. Most patients with mechanical ventilation have to receive sedative and analgesic drugs to reduce distress and oxygen consumption.[1–4]However, long periods of bed rest and restricted physical activity can result in ICU-acquired neuromuscular weakness, atelectasis, pressure ulcers, aspiration and pneumonia, muscle weakness and atrophy, bone mineral loss, orthostatic hypotension, tachycardia, and decreased cardiac output, which lead to significant impairment of physical function.[5–8]Recent studies[9–11]reported that early rehabilitation therapy is safe and feasible. But only few studies from China were reported, except a report about the effects of early rehabilitation therapy in patients with chronic obstructive pulmonary disease.[12]In this study, we investigated the feasibilityand effects of early rehabilitation therapy in mechanically ventilated patients of ICU, and compared with those of routine treatment.
METHODS
Patients
A randomized controlled trial was carried out. Sixty mechanically ventilated patients, with tracheal intubation or tracheostomy more than 48 hours and less than 72 hours, were admitted to the ICU of the Affiliated Hospital of Medical College, Qingdao University from May 2010 to May 2012. The institutional review board approved the study, and written informed consents were obtained from participants or their authorized representatives.
Patients in the ICU met the following criteria: 1) patient's age ≥18 years, duration of mechanically ventilation more than 48 hours but less than 72 hours, and duration of expected mechanically ventilation ≥1 week; 2) clear consciousness, cardiovascular stability (e.g., no postural hypotension, active cardiac ischemia, hypertension, or increasing infusion of vasopressor medication); 3) respiratory stability [e.g., stable oxygen saturation, fraction of inspired oxygen ≤55%, and positive end expiratory pressure (PEEP) ≤8 cmH2O]; 4) absence of an unstable fracture, for example, fracture of the cervical spine.
Patients were excluded for the following reasons: 1) inability to do activities independently (e.g., heading up actively, sitting, standing or ambulating), or require longterm mechanical ventilation before admission; 2) rapid development of neuromuscular disease, and irreversible disorders, with an estimated 6-month mortality of more than 50%; 3) increased intracranial pressure, absent limbs, preadmission glucocorticoids were applied for at least 20 days (prednisone >20 mg/d); 4) ICU admission after cardiopulmonary resuscitation; 5) tumor radiotherapy and chemotherapy within 6 months; 6) acute myocardial infarction or unstable ischemia within 3 weeks.
Procedures
Sixty patients met the inclusion criteria and were randomly assigned in a 1:1 ratio to the rehabilitation and control groups, 30 cases in each group. The primary diseases of patients at admission are shown in Table 1.
In the rehabilitation group, rehabilitation therapy was used twice daily, and the training time and intensity were adjusted according to the condition of the patients. Early rehabilitation therapy included heading up actively, transferring from the supine position to sitting position at the edge of the bed or sitting in chair, and from sitting to standing, and walking bedside.
Therapy was delivered at least by one physician and one nurse. At the time of the above-mentioned activities, the patients' position was changed every 2 hours, passively or actively. Progression of activities was dependent on patients' tolerance and stability. Therapy intervention continued on a daily basis throughout the patient's hospital stay until he or she returned to a previous level of function or was discharged. Initially with the assistance of a nurse or physician, the patients completed therapy independently gradually. Enteral nutrition was paused. The sedatives were used only at night if patients needed. If the patients needed sedation during the day, the medicine stopped 1–2 hours before rehabilitation training; when the patients were able to follow the instructions, rehabilitation continued. The patient's oxygen saturation and ECG were monitored during rehabilitation training in addition to blood pressure if necessary.
Rehabilitation termination criteria
The following criteria indicated unstable conditions that prevented the initiation or continuation of rehabilitation therapy: 1) mean arterial blood pressure<65 or >110 mmHg; heart rate <40 beats/min or >130 beats/min; respiratory rate <5 breaths/min or >40 breaths /min; and pulse oximetry <88%; 2) pale or sweaty and/or specifically request to stop because of acutely unwell. Serious adverse events included fall to knees, endotracheal tube removal, systolic blood pressure>200 mmHg, systolic blood pressure <90 mmHg, and desaturation to <80%, indwelling catheter prolapsed (such as enteral feeding tube, urinary tube, chest tube, arterial or venous catheters).
Statistical analysis
The patients' primary disease, body mass index, days to first out of bed, duration of mechanical ventilation, ICU length of stay, APACHE II score, highest FiO2,lowest PaO2/FiO2and hospital mortality of patients were compared between the rehabilitation and control groups. The differences between the two groups were compared using Student's t test.
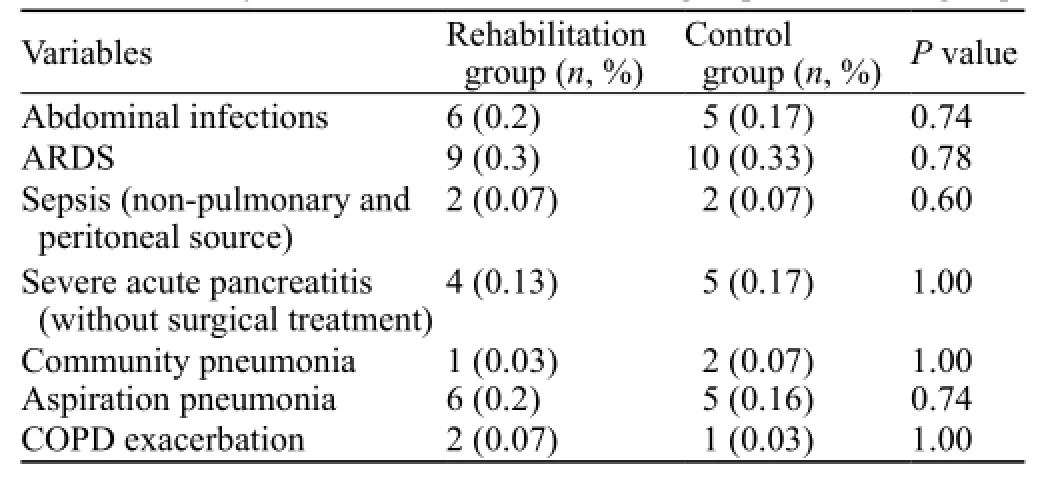
Table 1. Primary diseases of the rehabilitation group and control group
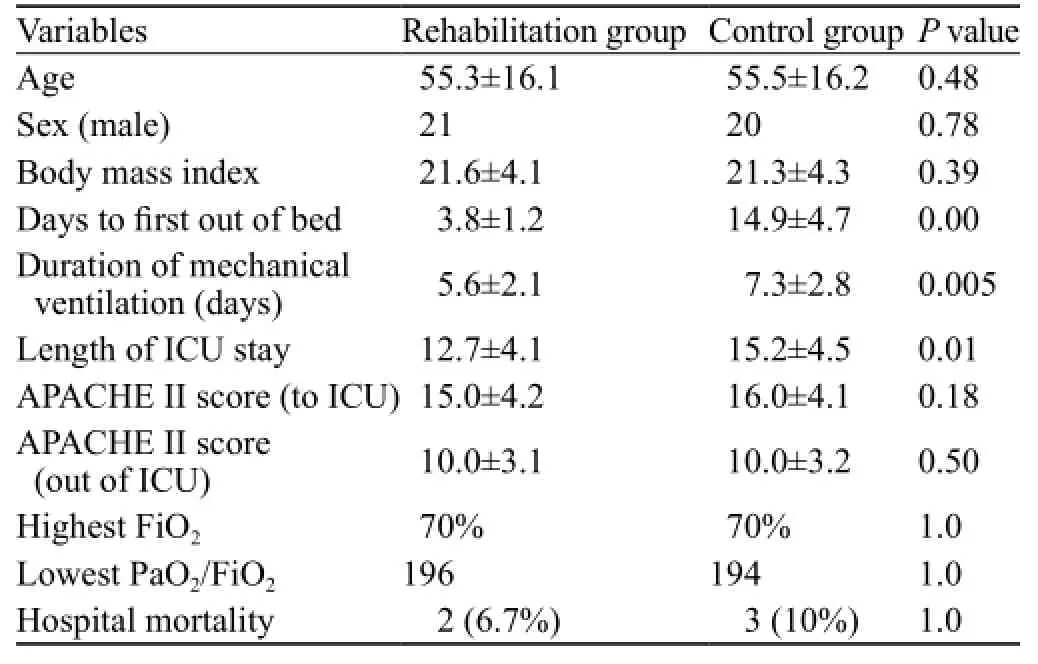
Table 2. Comparison of basic information between the rehabilitation and control groups
RESULTS
Comparison of primary diseases
Table 1 shows the baseline characteristics of the enrolled patients. There was no significant difference in primary disease between the rehabilitation and control groups (P>0.05).
Comparison of basic information
Table 2 shows the basic information of the enrolled patients. There was no significant difference in body mass index, APACHE II score, highest FiO2, lowest PaO2/FiO2and hospital mortality between the rehabilitation and control groups (P>0.05).
The first day out of bed, duration of mechanical ventilation and length of ICU stay were significantly shortened or reduced in patients from the rehabilitation group compared with the control group.
Two patients from the rehabilitation group and 3 patients from the control group died from complications after transferring to ordinary wards. No serious adverse events occurred in the rehabilitation group, and only 1 patient developed orthostatic hypotension when standing bedside, and blood pressure was quickly improved after taking a supine position.
DISCUSSION
Proper mechanical ventilation can improve pulmonary breathing, and reduce cardiac load.[13]But inevitably, mechanical ventilation can cause some side effects in hospitalized patients in ICU, especially in patients with neurological muscle weakness, known as ICU-acquired neuromuscular weakness. The etiology and pathogenesis of ICU-acquired neuromuscular weakness were associated with many factors.[14,15]Mechanical ventilation is one of the independent risk factors for death in trauma patients. Patients with a long duration of mechanical ventilation are prone to infection, myopathy and polyneuropathy.[16–18]In addition, high blood glucose and medications, such as neuromuscular blockers and corticosteroids, will induce the ICU-acquired neuromuscular weakness, and extend the duration of mechanical ventilation.[19–21]
ICU-acquired neuromuscular weakness may last a long time, and affect patients' life quality. Studies[22–24]showed that physiological function of survivors with mechanical ventilation was reduced, even lasted several years. Rehabilitation treatment usually begins after ICU discharge, while rehabilitation treatment may affect the follow up of the patients.
Currently, few studies reported the effects of early rehabilitation therapy on mechanical ventilation patients. In our study, early rehabilitation training was performed in accordance with the actual conditions of our hospital. No serious adverse events occurred in 30 patients of the rehabilitation group, except 1 patient with orthostatic hypotension after standing up. Our study proved that early rehabilitation is safe in the treatment of patients with mechanical ventilation.
The first day out of bed, duration of mechanical ventilation and length of ICU stay were significantly shortened or reduced in the rehabilitation group compared with the control group. Thus early rehabilitation therapy may improve patients' outcome as reported previously.
Between the rehabilitation treatment group and the control group, there was no significant difference in admission diagnosis, age, gender, body mass index, APACHE II score, FiO2, minimum and maximum PaO2/ FiO2. The use of continuous i.v. sedation was associated with the prolongation of mechanical ventilation in the ICU.[25,26]Daily interruption of sedation in critically ill patients with mechanical ventilation can result in a decreased duration of mechanical ventilation and a decreased length of ICU stay.[27]Deep sedation and immobility might potentiate ICU-acquired neuromuscular weakness.[28]Use of lighter sedation may reduce the rate of ICU-acquired neuromuscular weakness.[29–30]In this study, patients in the two groups were given daily interruption of sedation or no sedatives.On rehabilitation training, one nurse and one doctor were required to help the patients. The necessary equipment of early rehabilitation was also commonly used, so this mode could be widely replicated. Because of limitations, we didn't perform intensive training on patients, such as walking with ventilators. In other reports, walking distance can be up to 100 steps, even 212 steps, and this training could help patients wean from mechanical ventilation earlier.[31]
The results of this study cannot be directly applicable to all patients with mechanical ventilation, because the limitation of the sample size of participants, and it is not double blinded. Also, we lacked information about the follow-up of these patients out of ICU. In summary, this study suggested that early rehabilitation therapy is feasible, safe and effective in improving the outcomes of patients with mechanical ventilation, and the long-term efficacy of early rehabilitation therapy needs further study.
Funding:None.
Ethical approval:The study was approved by the Ethical Committee of the Affiliated Hospital of Medical College, Qingdao University, Qingdao, China.
Conflicts of interest:The authors declare that there is no conflict of interest.
Contributors:Dong ZH proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 Allen C, Glasziou P, Del MC. Bed rest: A potentially harmful treatment needing more careful evaluation. Lancet 1999; 354: 1229–1233.
2 Becher RD, Hoth JJ, Rebo JJ, Kendall JL, Miller PR. Locally derived versus guideline-based approach to treatment of hospital-acquired pneumonia in the trauma intensive care unit. Surg Infect (Larchmt) 2012; 13: 352–359.
3 Bruunsgaard H. Physical activity and modulation of systemic low-level inflammation. J Leukoc Biol 2005; 78: 819–835.
4 Convertino VA, Bloomfield SA, Greenleaf JE. An overview of the issues: physiological effects of bed rest and restricted physical activity. Med Sci Sports Exerc 1997; 29: 187–190.
5 Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, et al. Rehabilitation therapy and outcomes in acute respiratory failure: An observational pilot project. J Crit Care 2010; 25: 254–262.
6 Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated ,critically ill patients: a randomised controlled trial. Lancet 2009; 373: 1874–1882.
7 Needham DM. Mobilizing patients in the intensive care unit improving neuromuscular weakness and physical function. JAMA 2008; 300: 1685–1690.
8 Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 2008; 36: 2238–2243.
9 Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdjian L, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007; 35: 139–145.
10 Wu XY, Huang YZ, Liu HG, Huang DY, Tang R, Qiu HB. Effects of pulmonary stretch reflex on lung injury in rabbits with acute respiratory distress syndrome. World J Emerg Med 2011; 2: 296–301.
11 Hodgin KE, Nordon-Craft A, McFann KK, Mealer ML, Moss M. Physical therapy utilization in intensive care units: Results from a national survey. Crit Care Med 2009; 37: 561–567.
12 Shen M. Updated guidelines from pulmonary rehabilitation to see the progress of the study of pulmonary rehabilitation. Chin J Tuberc Respir Dis 2010; 33: 216–218.
13 Zhang JG, Chen XJ, Liu F, Zeng ZG, Qian KJ. Lung recruitment maneuver effects on respiratory mechanics and extravascular lung water index in patients with acute respiratory distress syndrome. World J Emerg Med 2011; 2: 201–205.
14 Hough CL. Neuromuscular sequelae in survivors of acute lung injury. Clin Chest Med 2006; 27: 691–703.
15 Maramattom BV, Wijdicks EF. Acute neuromuscular weakness in the intensive care unit. Crit Care Med 2006; 34: 2835–2841.
16 Ciesla DJ, Moore EE, Johnson JL, Cothren CC, Banerjee A, Burch JM, et al. Decreased progression of postinjury lung dysfunction to the acute respiratory distress syndrome and multiple organ failure. Surgery 2006; 140: 640-647. Epub 2006 Aug 30.
17 Morin AM, Zähringer J, Kasper M, von Schmädel E, Suhayda A. Acute respiratory insufficiency after inhaling concrete dust—a case report. Anasthesiol Intensivmed Notfallmed Schmerzther 1997; 32: 56–60.
18 Tellez PA, Pronovost PJ, Needham DM. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med 2007; 33: 1876–1891.
19 Hermans G, Wilmer A, Meersseman W, Milants I, Wouters PJ, Bobbaers H, et al. Impact of intensive insulin therapy on neuromuscular complications and ventilator dependency in the medical intensive care unit. Am J Respir Crit Care Med 2007; 175: 480–489. Epub 2006 Nov 30.
20 Larsson L, Li X, Edström L, Eriksson LI, Zackrisson H, Argentini C, et al. Acute quadriplegia and loss of muscle myosin in patients treated with nondepolarizing neuromuscular blocking agents and corticosteroids: mechanisms at the cellular and molecular levels. Crit Care Med 2000; 28: 34–45.
21 De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, et al. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 2002; 288: 2859–2867.
22 Chu YF, Jiang Y, Meng M, Jiang JJ, Zhang JC, Ren HS, et al. Incidence and risk factors of gastrointestinal bleeding in mechanically ventilated patients. World J Emerg Med 2010; 1: 32–36.
23 Orme J Jr, Romney JS, Hopkins RO, Pope D, Chan KJ, Thomsen G, et al. Pulmonary function and health-related quality of life in survivors of acute respiratory distresssyndrome. Am J Respir Crit Care Med 2003; 167: 690–694.
24 Curtis JR. The long-term outcomes of mechanical ventilation: What are they and how should they be used? Respir Care 2002; 47: 496–505.
25 Ostermann ME, Keenan SP, Seiferling RA, Sibbald WJ. Sedation in the intensive care unit: a systematic review. JAMA 2000; 283: 1451–1459.
26 Kollef MH, Levy NT, Ahrens TS, Schaiff R, Prentice D, Sherman G. The use of continuous i.v. sedation is associated with prolongation of mechanical ventilation. Chest 1998; 114: 541–548.
27 Kress JP, Pohlman AS, O'Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med 2000; 342: 1471–1477.
28 Huang H, Xu XH, Chen Y, Lu LX, Zhu CQ. Early tracheotomy for acute severe asthma. World J Emerg Med 2011; 2: 154–156.
29 De Jonghe B, Bastuji-Garin S, Fangio P, Lacherade JC, Jabot J, Appéré-De-Vecchi C, et al. Sedation algorithm in critically ill patients without acute brain injury. Crit Care Med 2005; 33: 120–127.
30 Schweickert WD, Gehlbach BK, Pohlman AS, Hall JB, Kress JP. Daily interruption of sedative infusions and complications of critical illness in mechanically ventilated patients. Crit Care Med 2004; 32: 1272–1276.
31 Martin UJ, Hincapie L, Nimchuk M, Gaughan J, Criner GJ. Impact of whole-body rehabilitation in patients receiving chronic mechanical ventilation. Crit Care Med 2005; 33: 2259–2265.
Received April 22, 2013
Accepted after revision September 10, 2013
World J Emerg Med 2014;5(1):48–52
10.5847/ wjem.j.issn.1920–8642.2014.01.008



