Mount Sinai Medical Center, Department of Emergency Medicine, Miami Beach, FL 33140, USA
Corresponding Author:Daniel M. Aronovich, Email: danaronuf@gmail.com
Cushing's reflex in a rare case of adult medulloblastoma
Daniel Aronovich, Alexander Scumpia, David Edwards
Mount Sinai Medical Center, Department of Emergency Medicine, Miami Beach, FL 33140, USA
Corresponding Author:Daniel M. Aronovich, Email: danaronuf@gmail.com
BACKGROUND:Medulloblastoma is a primitive neuro-ectodermal tumor. It is common in childhood, but rarely seen at adult age, comprising only 1% of primary brain tumors.
METHODS:We treated a 31-year-old man presented to the emergency department (ED) with a chief complaint of nausea and vomiting for one week duration. Immediate frozen section revealed a grade IV medulloblastoma. During the hospital course, the patient was given craniospinal irradiation with chemotherapy.
RESULTS:The patient was eventually discharged from the hospital to an assisted living facility after an uneventful 15-day course with the aid of social work.
CONCLUSIONS:Despite intracranial tumors generally being slow growing masses, this patient demonstrates how quickly one can decompensate, and how important it is to recognize these clinical signs and symptoms of an intracranial lesion. Although these symptoms (i.e. Cushing response) are extremely rare, the ED physician should be aware and appreciate their clinical signi fi cance.
Medulloblastoma; Adualt; Cushing's re fl ex
INTRODUCTION
M edulloblastoma is a primitive neuro-ectodermal tumor. It is common in childhood, but rarely seen at adult age, comprising only 1% of primary brain tumors.[1]There are not many studies concerning the treatment of these tumors. Medulloblastomas most commonly present with signs of increased intracranial pressure, including nocturnal or morning headaches, nausea, vomiting, and altered mental status. Treatment involves maximal surgical resection, craniospinal irradiation, and chemotherapy. Approximately 70% of the patients have a long-term survival rate but usually at the cost of signi fi cant neurocognitive impairment.[2]
CASE REPORT
A 31-year-old man presented to the emergency department (ED) with a chief complaint of nausea and vomiting for one week duration. He reported being homeless and eating out of the garbage for nutrition. The patient also stated several episodes of non-bloody, non-bilious emesis not associated with abdominal pain. The remainder of his review of symptoms was grossly unremarkable. Initial ED vital signs were: blood pressure 135/87 mmHg, pulse 53 beats per minute, oral temperature 97 degrees Fahrenheit, respiratory rate 20 breaths per minute, and pulse oximetry 99 percent on room air. Physical exam demonstrated a disheveled but pleasant young man in no apparent distress with dry mucus membranes. Additionally, he had clear breath sounds, a slow, regular heart rate without murmurs, rubs or gallops, a soft, non-tender, non-distended abdomen, and no gross focal neurologic deficits. The patient was treated for a presumed case of food poisoning with ondansetron, intravenous fl uids and discharged.
Later that same evening, the patient returned to the emergency room with a new chief complaint of dizziness and difficulty ambulating. His vital signs were as follows: blood pressure 144/88 mmHg, pulse 42 beats per minute, oral temperature 98.1 degrees Fahrenheit, respiratory rate 16 breaths per minute, and pulse oximetry 99 percent on room air. The patientshowed nauseous and ill appearance. Repeat neurological exam demonstrated impressive dysmetria, a positive Romberg sign, and most signi fi cantly, a wide, unsteady, slowed gait. ED non-contrast computed tomography of the brain demonstrated a 5.1 cm left cerebellopontine angle mass with significant obstructive hydrocephalus and bilateral cerebellar tonsillar herniation (Figures 1–3). Neurosurgery was emergently consulted and treatment was recommended with IV dexamethasone and furosemide. Repeat vital signs showed a blood pressure of 180/100 mmHg, a pulse 39 beats per minute and a respiratory rate of 10 shallow breaths per minute. Due to the patient's rapid clinical decompensation, the patient was taken for an emergent ventriculostomy and left posterior fossa craniectomy for subtotal resection of the mass. Immediate frozen section revealed a grade IV medulloblastoma. During the hospital course, the patient was given craniospinal irradiation with chemotherapy, and was eventually discharged from the hospital to an assisted living facility after an uneventful 15-day course with the aid of social work.
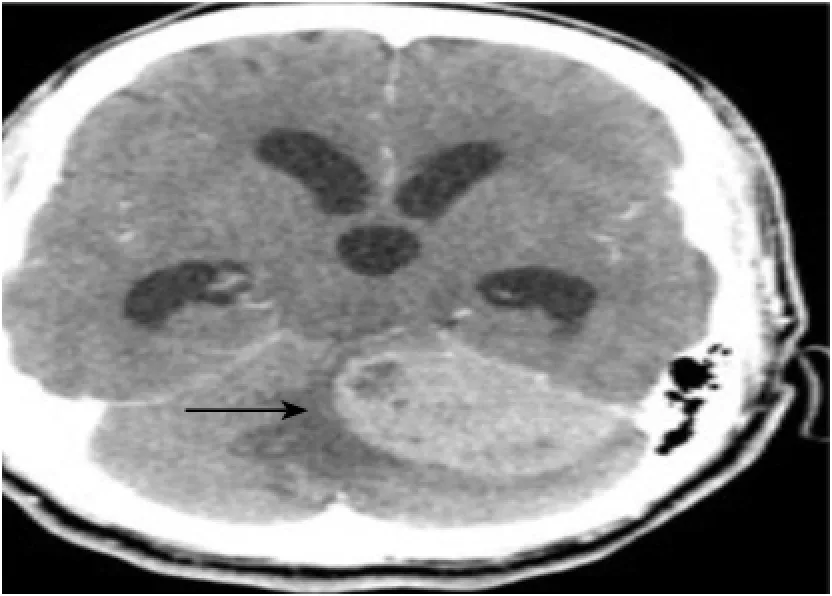
Figure 1. Brain CT (axial view) demonstrating a left cerebellopontine mass with distention of the third ventricle, the frontal and the temporal horns of the lateral ventricles.

Figure 2. Brain CT (saggital view) demonstrating a left cerebellopontine mass with distention of the frontal horns of the lateral ventricles.
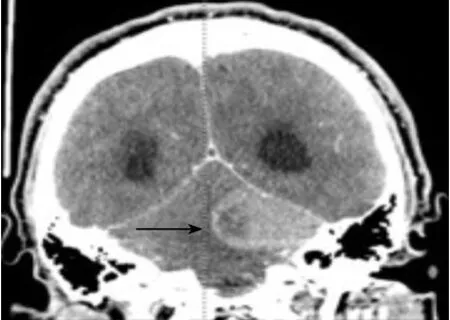
Figure 3. Brain CT (coronal view) demonstrating a left cerebellopontine mass with cystic versus necrotic areas and surrounding vasogenic edema.
DISCUSSION
Medulloblastoma is the most common malignant brain tumor of childhood (among children aged less than 19 years ), accounting for approximately 20% of all primary tumors of the central nervous system.[1]The incidence peaks at 5–9 years of age and approximately 70% of the patients are diagnosed before the age of 20 years. Interestingly, there is a slight increase in the incidence between 20–24 years of age, and the tumor is extremely rare after the fourth decade. Furthermore, medulloblastoma accounts for only 1% of all primary brain tumors in adults, a fi nding which may be attributed to the embryonal origin of the tumor.[1]Anatomically, these tumors classically arise in the cerebellar midline in children and more laterally in the cerebellar hemispheres in adults.[3]Medulloblastoma clinically presents with signs of increased intracranial pressure, secondary to mass effect blocking drainage through the 4th ventricle. Signs of increased intracranial pressure are usually present 1 to 5 months prior to diagnosis.[4]The initial symptoms can include repeated episodes of vomiting or morning headache, but can develop ataxia, stumbling gait and frequent falls. Head titubation (or head bobbing), nystagmus, facial sensory loss, and diplopia secondary to sixth cranial nerve palsy may also be present.[4]Treatment involves gross neurosurgical resection and may additionally include craniospinal irradiation with adjuvant chemotherapy with agents such as cisplatin, lomustine, cyclophosphamide, and vincristine.[2]The majority of patients have a favorable 5-year survival, but with signi fi cant neurocognitive impairment and sequelae.[5]
There are three clinically interesting findings in this case. First, medulloblastoma diagnosed in an adult is a rare occurrence. Second, it is rare for a patient to escape the surgical and postsurgical management of amedulloblastoma without any serious neurocognitive impairment. Third, this patient exhibited Cushing's triad, a rare clinical finding. The Cushing response, or "re fl ex", as fi rst described by Dr. Harvey Cushing in the early 1900s manifests as a result of an abrupt increase in intracranial pressure.[6]It consists of the classical triad of hypertension, bradycardia, and slow, irregular breathing elicited by the stimulation of mechanically sensitive regions in the paramedian caudal medulla. The proximate cause of the Cushing response is an anatomical distortion of the lower brain stem. This can be either from a mass in the posterior fossa, or more often, from a large mass in one of the hemispheres causing a transmitted pressure that compresses the fourth ventricle.[6]Initial emergency treatment strategies include: elevating the head of the bed 30 degrees, osmotic diuretics such as mannitol and furosemide, short-term hyperventilation, steroids, or cerebrospinal drainage via ventriculostomy.[5–8]
In conclusion, despite intracranial tumors generally being slow growing masses, this patient demonstrates how quickly one can decompensate, and how important it is to recognize these clinical signs and symptoms of an intracranial lesion. Although these symptoms (i.e. Cushing response) are extremely rare, the ED physician should be aware and appreciate their clinical signi fi cance.
Funding:None.
Ethical approval:This study was approved by the institutional ethics Committees.
Con fl icts of interest:We have no con fl icts of interest to report.
Contributors:Aronovich D proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
1 Brandes AA, Palmisano V, Monfardini S. Medulloblastoma in adults: clinical characteristics and treatment. Cancer Treat Rev 1999; 25: 3–12.
2 Ropper AH, Samuels MA. Chapter 31. Intracranial Neoplasms and Paraneoplastic Disorders. In: Ropper AH, Samuels MA, eds. Adams and Victor's Principles of Neurology. 9th ed. New York: McGraw-Hill; 2009. http://www.accessmedicine.com/content. aspx?aID=3637579. Accessed February 10, 2013.
3 DeAngelis LM, Wen PY. Chapter 379. Primary and Metastatic Tumors of the Nervous System. In: Longo DL.
4 Hoffman BB, Taylor P: Neurotransmission: The autonomic and somatic motor nervous systems, in Hardman JG, Limbird LE (eds): Goodman and Gilman's The Pharmacological Basis of Therapeutics, 10th ed. New York, McGraw-Hill, 2001: 115–153.
5 Francony G, Fauvage B, Falcon D, Canet C, Dilou H, Lavagne P, et al. Equimolar doses of mannitol and hypertonic saline in the treatment of increased intracranial pressure. Crit Care Med 2008; 36: 795.
6 Stocchetti N, Maas AI, Chieregato A, van der Plas AA. Hyperventilation in head injury: a review. Chest 2005; 127: 1812.
7 Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J, eds. Harrison's Principles of Internal Medicine. 18th ed. New York: McGraw-Hill; 2012. http://www.accessmedicine.com/content. aspx?aID=9147519. Accessed March 8, 2013.
8 Hoff JT, Reis DJ. Localization of regions mediating the Cushing response in CNS of cat. Arch Neurol 1970; 23: 228–240.
Received September 23, 2013
Accepted after revision April 6, 2014
World J Emerg Med 2014;5(2):148–150
10.5847/ wjem.j.issn.1920–8642.2014.02.013



