Department of Anesthesia, School of Medicine, Gondar College of Medicine and Health Sciences, University of Gondar, Gondar 196, Ethiopia
Corresponding Author:Endale Gebreegziabher Gebremedhn, Email: endalege@yahoo.com
Knowledge and skills of neonatal resuscitation of health professionals at a university teaching hospital of Northwest Ethiopia
Endale Gebreegziabher, Adugna Aregawi, Habtamu Getinet
Department of Anesthesia, School of Medicine, Gondar College of Medicine and Health Sciences, University of Gondar, Gondar 196, Ethiopia
Corresponding Author:Endale Gebreegziabher Gebremedhn, Email: endalege@yahoo.com
BACKGROUND:Competency in neonatal resuscitation is critical in the delivery rooms, neonatology units and pediatrics intensive care units to ensure the safety and health of neonates. Each year, millions of babies do not breathe immediately at birth, and among them the majority require basic neonatal resuscitation. Perinatal asphyxia is a major contributor to neonatal deaths worldwide in resource-limited settings. Neonatal resuscitation is effective only when health professionals have sufficient knowledge and skills. But malpractices by health professionals are frequent in the resuscitation of neonates. The present study was to assess the knowledge and skills of health professionals about neonatal resuscitation.
METHODS:An institution based cross-sectional study was conducted in our hospital from February15 to April 30, 2014. All nurses, midwives and residents from obstetrics-gynecology (obsgyn), midwifery and pediatric departments were included. The mean scores of knowledge and skills were compared for sex, age, type of profession, qualification, year of service and previous place of work of the participants by using Student's t test and ANOVA with Scheffe's test. A P value <0.05 was considered statistically signi fi cant.
RESULTS:One hundred and thirty-five of 150 participants were included in this study with a response rate of 90.0%. The overall mean scores of knowledge and skills of midwives, nurses and residents were 19.9 (SD=3.1) and 6.8 (SD=3.9) respectively. The mean knowledge scores of midwives, nurses, pediatric residents and obs-gyn residents were 19.7 (SD=3.03), 20.2 (SD=2.94), 19.7 (SD=4.4) and 19.6 (SD=3.3) respectively. Whereas the mean scores of skills of midwives, nurses, pediatric residents and obs-gyn residents were 7.1 (SD=4.17), 6.7 (SD=3.75), 5.7 (SD=4.17) and 6.6 (SD=3.97) respectively.
CONCLUSIONS:The knowledge and skills of midwives, nurses and residents about neonatal resuscitation were substandardized. Training of neonatal resuscitation for midwives, nurses and residents should be emphasized.
Neonatal resuscitation; Knowledge; Skill; Health professionals
INTRODUCTION
Neonatal deaths are the major obstacles for the improvement of survival of under five children in developing countries.[1]An estimated 4 million babies die in the neonatal period yearly and approximately all of these deaths occur in low- and middle-income countries.[2,3]The need for information on neonatal deaths is increasing because of an increase in the percentage of mortalitywith a current report of about 40% of global under-five mortality occurs in the neonatal period.[4]
World Health Organization defined birth asphyxia as failure to initiate and sustain breathing at birth.[5]Every newborn should be considered at a high risk of birth asphyxia since most cases of asphyxia cannot be predicted.[6]Although neonatal death is multifactorial, the most important single causes of neonatal deaths were preterm birth, birth asphyxia, sepsis and pneumonia.[7–9]According to 2012 UN inter-agency group report for child mortality estimation, slower reductions in neonatal mortality than in under-five mortality were seen in all regions over the past 22 years.[10]
A study conducted in Nigeria showed that the common cause for neonatal deaths were prematurity and perinatal asphyxia.[11]Other studies[12–14]from Nigeria and Malawi found that the main cause for neonatal death was birth asphyxia, indicating that the skills of health professionals about neonatal resuscitation was very crucial to immediate neonatal outcome.
A study[15]conducted in Kenya showed that more than 70% of the health professionals considered that their knowledge about neonatal resuscitation was inadequate because of inadequate medical training. Similarly, a study from Western Nigeria found that the knowledge of nurses about neonatal resuscitation was poor.[16]
Although all health professionals were given training about neonatal resuscitation during their undergraduate courses, we found malpractices of neonatal resuscitation in our hospital. The aim of this study was to assess the knowledge and skills of health professionals about neonatal resuscitation.
METHODS
Study design and participants
An institution-based cross-sectional study was conducted in our teaching and referral hospital from February15 to April 30, 2014.
All midwives, nurses and residents from obs-gyn, pediatric and midwifery departments during the study period were included;whereas those individuals who were sick during the data collection time were excluded.
Operational de fi nitions
Health professionals included midwives, nurses and residents. Midwives were those who worked in the obsgyn and midwifery departments. Nurses included those who worked in the pediatric department. Residents included physicians who were on postgraduate study in obs-gyn and pediatric departments.
Study tools
A structured questionnaire was developed addressing socio-demographic, theoretical and practical aspects of the knowledge and skills of the participants about basic life support (BLS) and advanced cardiac life support (ACLS) based on the 2010 United Kingdom (UK) Resuscitation Council Guidelines. The questionnaire was validated and pilot tested in other hospitals and changes were made before the study. Forty-six questions used to assess knowledge and each correct answer was given one point. The knowledge level of midwives, nurses and residents was classi fi ed as suf fi cient for midwives, nurses and residents who answered correctly at least 37 of the 46 questions (total score of >80%) and insufficient for midwives, nurses and residents who correctly answered for less than 37 of the 46 questions (total score <80%) according to the 2005 American Heart Association (AHA) accreditation criteria.
Whereas 12 questions were used to assess the skills and each correct answer was given one point. The skills of the midwives, nurses and residents were classified as sufficient for midwives, nurses and residents who answered correctly at least 10 of the 12 questions (total score of >80%) and insuf fi cient for midwives, nurses and residents who correctly answered less than 10 of the 12 questions (total score <80%) according to the 2005 AHA accreditation criteria.
Data collection procedures
The authors distributed the self administered questionnaires to the participants in the respective departments.
Data processing and analysis
The data were coded, entered and analyzed using SPSS version 20 software. The mean scores of knowledge and skills were compared for sex, age, type of profession, quali fi cation, year of experience and previous places of work of the participants by using Student's t test and ANOVA with Scheffe's test. A P value <0.05 was considered statistically signi fi cant.
Ethical considerations
Ethical clearance was obtained from the institutional ethical review board of our university. Informed consent was obtained from each participant after explanation of what study they will be involved in. Con fi dentiality was ensured by using an anonymous questionnaire.
RESULTS
Socio-demographic characteristics of the participants
Altogether 150 participants were from the midwifery, obs-gyn and pediatric departments of the hospital. Eight participants were excluded because of the incomplete questionnaires and 7 participants refused to participate in the study. One hundred and thirty-five of the 150 participants were included in this study with a response rate of 90.0%. Males accounted for 58.5% of the participants. The minimum, maximum and median ages of the participants were 19, 50 and 26.0 years respectively. Of the participants, 51 (37.8%), 53 (39.3%), 11 (8.1%), and 20 (14.8%) were midwives, nurses, pediatric residents and obs-gyn residents, respectively.
In the 135 participants, 8 (5.9%), 87 (64.4%), 9 (6.7%), 7 (5.2%), 9 (6.7%), 14 (10.4%), and 1 (0.7%) were diploma holders, BSc holders, MSc holders, first year residents, second year residents, third year residents and fourth year residents, respectively. The periods of experience of 26 (19.3%), 39 (28.9%), 34 (25.2%) and 36 (26.7%) participants were < 1 year, 1–3 years, 4–5 years and > 5 years, respectively. The places of previous work of 73 (54.1%), 20 (14.8%), 24 (17.8%) and 18 (13.3%) of the participants were the University of Gondar, district hospital, other teaching hospital, and district clinic, respectively.
Knowledge levels of health professionals about neonatal resuscitation
The minimum and maximum knowledge scores of health professionals (midwives, nurses and residents) were 13 and 27 (IQR=4) respectively. The overall mean knowledge score about neonatal resuscitation in health professionals was 19.9 (SD=3.1). The mean knowledge scores of midwives, nurses, pediatrics residents and obsgyn residents were 19.7 (SD=3.03), 20.2 (SD=2.94), 19.7 (SD=4.4) and 19.6 (SD=3.3) respectively. The overall knowledge about neonatal resuscitation in health professionals was poor (<80%).
The correct responses given by midwives were more than 50% for only 13 of 46 knowledge questions. Of these questions, the percentages of correct responses were > 80% for five questions. The percentages of responses ranged from 50% to 79% for 8 questions. On the other hand, the percentage of correct responses for 33 questions was <50% (Table 1).
The correct response given by nurses was more than 50% for 16 of the 46 knowledge questions. Of these questions, the percentage of correct responses was > 80% for 3 questions; wiping meconium from the face and nose while the head appears before delivery is important to prevent aspiration (43, 81.1%). If the baby is not breathing after full delivery, the mouth and nose should be suctioned before drying and stimulating (47, 88.7%) and face mask should cover the nose, mouth and chin during mask ventilation (46, 86.8%).
On the other hand, the correct response was in the range of 50%–79% for 13 questions. The nose followed by the mouth should be suctioned as soon as the head is at the perineum before shoulder delivery to prevent aspiration (34, 64.2%). The baby should be placed on the abdomen of the mother in skin to skin contact and be covered with fresh, dry linen to prevent hypothermia (41, 77.4%). During suctioning, the catheter should be placed in the mouth and nose before turning on thedevice (35, 66.0%). Effective mask ventilation (34, 66.7%) was confirmed, and measures were taken for dif fi cult mask ventilation (39, 73.6%). Ventilation should be commenced within one minute for newborns who have no breathing efforts immediately after delivery (37, 69.8%). The commonest cause for cardiac arrest in children (38, 71.7%), the depth of chest compression in neonates during CPR (32, 60.4%), the commonest arrhythmia in children (33, 62.3%), the dose of adrenaline for neonates during CPR (27, 50.9%), and the dose of amiodarone for neonates during CPR (31, 58.5%) were considered when adrenaline was given during CPR for neonates and children (29, 54.7%). The heart rate <60 bpm was considered as a sign of cardiac arrest for neonates and infants (27, 50.9%). The percentage of correct responses given by nurses was less than 50% for 30 questions.
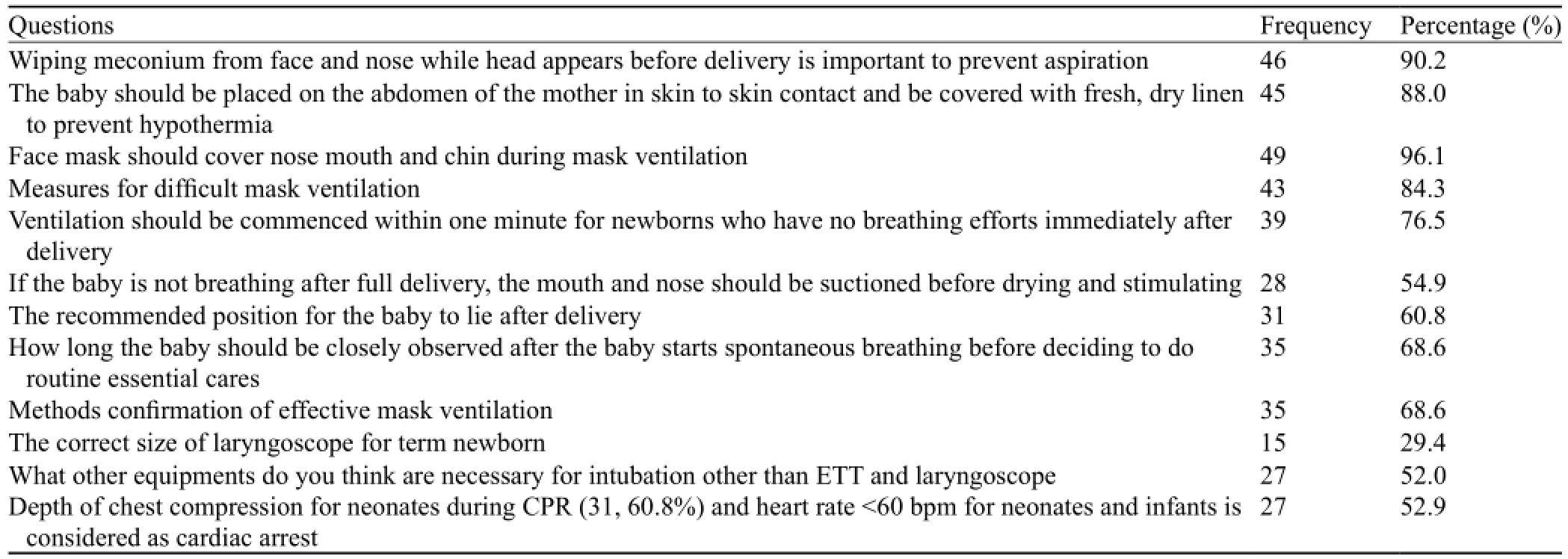
Table 1. Correct responses to knowledge questions by midwives
The percentage of correct responses given by pediatric residents was more than 50% for 21 of the 46 questions.The percentage of correct responses was >80% for 9 questions. Wiping meconium from the face and nose while the head appears before delivery is important to prevent aspiration (10, 90.9%). Whether the baby starts spontaneous breathing after delivery (11, 100%) is decided. If the baby is not breathing after full delivery, his/her mouth and nose should be suctioned before drying and stimulating (9, 81.8%). Effective mask ventilation was performed (9, 81.8%), and measures were taken for difficult mask ventilation (10, 90.9%). The commonest cause for cardiac arrest was seen in children (11, 100%), and the depth of chest compression was detected in neonates during CPR (11, 100%). The dose of adrenaline was de fi ned during CPR for neonates (10, 90.9%) and how much fluid should be given if hypotension is suspected for newborns (10, 90.9%). The percentage of correct responses was <50% for 25 questions.
Of the 46 questions, the percentage of correct responses given by obs-gyn residents was >50% for 24 questions. The percentage of correct responses was >80% for 6 questions. The baby should be placed on the abdomen of the mother in skin to skin contact and be covered with fresh, dry line to prevent hypothermia (17, 85%). Measures were taken for dif fi cult ventilation (17, 85%), and ventilation should be performed within one minute for newborns who have no breathing efforts immediately after delivery (16, 80%). The commonest cause of cardiac arrest in children (16, 80%), the depth of chest compression in neonates during CPR (16, 80%) and the ratio of chest compression to ventilation for newborns were observed during CPR (17, 85%).
On the other hand, the percentage of correct responses given by obs-gyn residents was in the range of 50%–79% for 18 questions. The percentage of correct responses was <50% for 22 questions (Table 2).
Skills of health professionals about neonatal resuscitation
The minimum and maximum scores of skills of health professionals (midwives, nurses, pediatricresidents and obs-gyn residents) were 0 and 17 (IQR=6) respectively. The overall mean skill score of health professionals about neonatal resuscitation was 6.8 (SD=3.9). The mean skill scores of midwives, nurses, pediatrics residents and obs-gyn residents were 7.1 (SD=4.17), 6.7 (SD=3.75), 5.7 (SD=4.17) and 6.6 (SD=3.97) respectively. The overall skill of health professionals about neonatal resuscitation was poor (<80%).
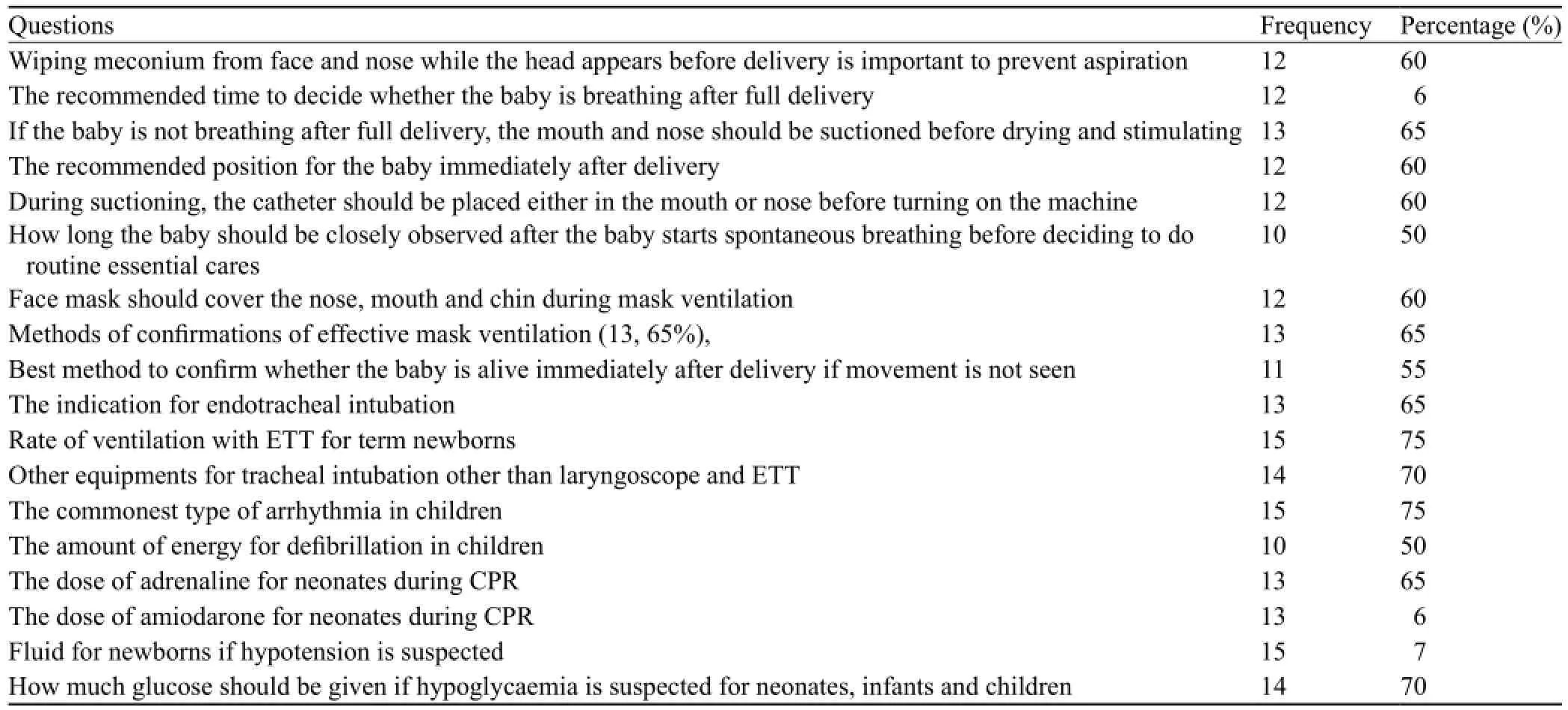
Table 2. Correct responses given by obs-gyn residents for knowledge questions
The percentage of correct responses given by midwives was >50% for only two questions of 12 skill questions, i.e., have you attended CPR session in your curriculum (26, 50.9%) and the time since last neonatal resuscitation attempt (38, 74.5%). The percentage of correct responses was <50% for 10 questions.
The percentage of correct responses given by nurses was > 50 % for 3 of 12 skill questions, i.e., time since the last training (27, 50.9%), the number of attempted real CPR cases on neonates (27, 50.9%), and time since the last neonatal resuscitation attempt (31, 58.5%). The percentage of correct responses was <50% for 9 questions.
The percentage of correct responses given by pediatrics residents was >50% for 5 of 12 skill questions. The percentage of correct responses was >80% for 2 questions, i.e., the number of attempted real CPR cases on neonates (10, 90.9%) and have you performed chest compression on a collapsed neonate (9, 81.8%). On the other hand, the percentage of correct responses was in the range of 50%–79% for three questions: time since you attended your last course on neonatal resuscitation (2, 54.55); have you participated in CPR session other than in the curriculum (7, 63.6%); and time since the last neonatal resuscitation attempt (7, 63.6%). The percentage of correct responses was <50% for 7 questions.
The percentage of correct responses given by obsgyn residents was > 50% for 6 of 12 skill questions. Of these, the percentage of correct responses was > 80% for three questions: the number of attempted real CPR cases on neonates (19, 95%); time since the last neonatal resuscitation attempt (19, 95%), and have you performed chest compression on a collapsed neonate (18, 90%). In addition, the percentage of responses was in the range of 50%–79% for three questions: time since you attended your last CPR course on neonatal resuscitation (11, 55%); have you been a team leader during CPR (10, 50%); and have you intubated a neonate with an endotracheal tube (12, 60%). The percentage of correct responses was <50% for 6 questions.
Comparison of knowledge scores in relation to the different characteristics of the
participants
There was no signi fi cant difference in the knowledge score of the participants in terms of age (P=0.303), type of profession (P=0.847), quali fi cation (P=0.055), year of service (P=0.391) and place of previous work (P=0.209) (Table 3).
From the independent t-test, the mean knowledge score was significantly different in terms of sex of the participants (male vs. female, P=0.024) (Table 4).
Comparison of skill scores in relation to the different characteristics of the participants
There was no signi fi cant difference in skill scores of the participants in terms of sex (P=0.139), age (P=0.372), type of profession (P=0.769), year of service (P=0.121), qualification (P=0.340) and place of previous work (P=0.214) (Table 5).
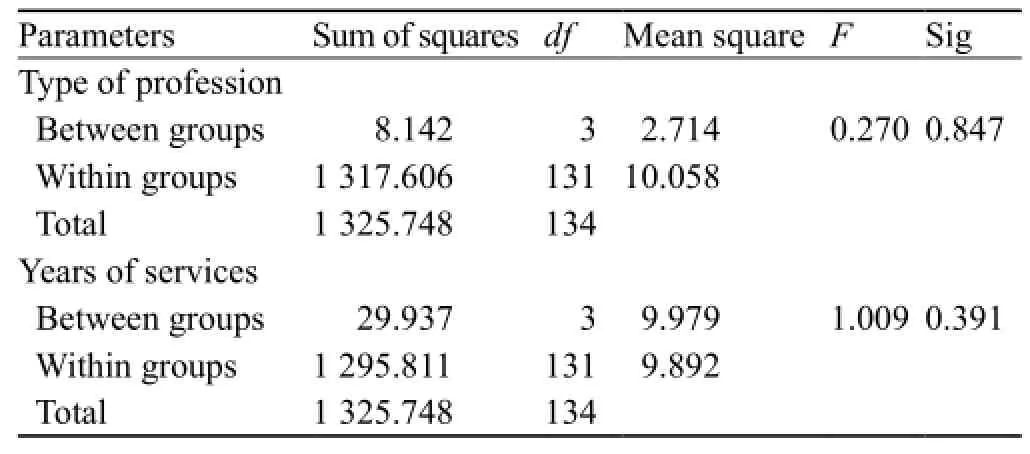
Table 3. Comparison of knowledge scores in terms of type of profession and year of services, ANOVA test (n=135)
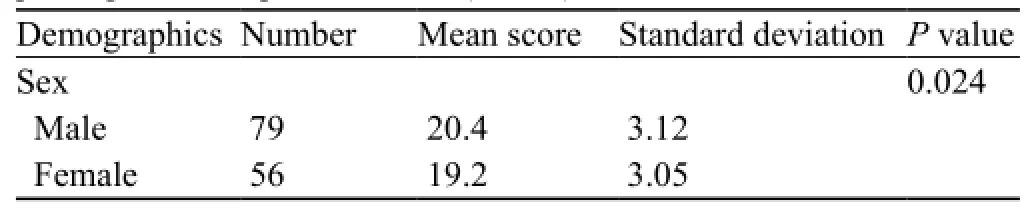
Table 4. Comparison of knowledge scores in terms of sex of the participants, independent t-test (n=135)
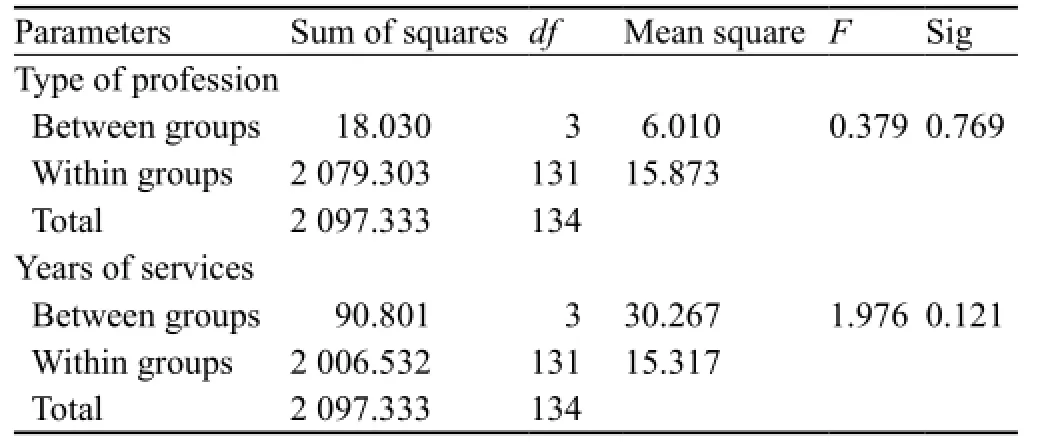
Table 5. Comparison of skill scores in terms of type of profession and year of services, ANOVA test (n=135)
DISCUSSION
This study showed that the overall knowledge and skills of midwives, nurses, pediatrics residents, and obs-gyn residents were insufficient. The overall mean knowledge and skill scores of health professionals (midwives, nurses and residents) were 19.9 (SD=3.1) and 6.8 (SD=3.9) respectively.
In this study, the mean knowledge score of midwives was poor (42.8%). This fi nding was in line with a study from Ghana (38%).[17]This might be due to lack of exposure to an adequent number of real cardiopulmonary resuscitation cases, simulation-based training, updating training, and certi fi cation process before graduation.
The mean knowledge score of nurses was poor (43.9%). This finding was in agreement with the same study from Ghana (43.9%).[17]The low level of performance could be due to limited exposure to real cardiopulmonary resuscitation cases during the undergraduate course, lack of certification processes before leaving the university and updating training.
The mean knowledge score of pediatric residents was poor (42.8%). The finding was in sharp contrast to the result of a study from Khartoum University, Sudan (51.9%).[19]This difference in the score might be due to the difference in the quality of the training given to the residents and the facilities available.
In our study, the mean knowledge score of obs-gyn residents was very low (42.6%). This score was lower than that of a study of India (69.1%).[20]The discrepancy could be due to the difference in the quality of training on neonatal resuscitation and the facilities available for neonatal resuscitation.
The mean knowledge score of men was different and higher than women (men vs. women, 20.4 vs. 19.2, P=0.024). This could be probably because women might not actively participate in the resuscitation activities since there are cultural in fl uences where most women are reserved to be involved in different occasions especially in developing countries like Ethiopia. Even if it is statistically significant, it is still difficult to generalize since our sample size was small.
In our study, the mean skill score of midwives was poor (59.2%). This finding was not consistent with a study conducted in Afghanistan.[18]This discrepancy might be due to the availability of simulation-based training, updating training, and certification process before graduation in Afghanistan which is not existed in our case.
The mean skill score of nurses was poor (55.8%). Our finding was similar to that in a study conducted in Western Nigeria (59.8%).[16]This might be due to the absence of standardized training during the undergraduate and postgraduate courses.
The mean skill score of pediatric residents was insufficient (47.5%). This finding was consistent with the result in a study from Iran (52%).[21]The low skill level of the residents might be due to lack of training during their undergraduate and postgraduate study. In our study, the percentage of their responses to skill questions was >80% for two questions, 50%–79% for three questions, and <50% for seven questions. Only 4 (36.4%) residents attended CPR sessions in their curriculum, 3 (27.3%) attended 1–5 real CPR sessions, and 7 (63.6%) attended greater than 5 real CPR sessions during the undergraduate course. Four (36.4%) residents got technical training in intubation and no resident de fi brillated on a collapsed neonate or intubated neonate.
The mean skill score of obs-gyn residents was substandardized (55%). This finding was in agreement with a study from Iran (52%).[21]This could be due to inadequate training of obs-gyn residents about neonatal resuscitation during their undergraduate and postgraduate courses. In our study, the percentage of their response to skill questions was >80% for three questions, 50%–79% for three questions and <50% for six questions. Only 8 (40%) residents attended CPR sessions in their curriculum, 7 (35%) attended 1–5 real CPR sessions and 12 (60%) attended greater than 5 real CPR sessions during their undergraduate courses. Three (15%) residents got technical training in intubation None of the residents de fi brillated on a collapsed neonate and 7 (35%) intubated neonates.
In conclusion, the knowledge and skill levels of midwives, nurses, pediatrics residents and obs-gyn residents about neonatal resuscitation were substandardized. There was no significant difference in the knowledge and skill scores of the participants in terms of sex (except knowledge), age, type of profession, qualification, year of services and previous place of work, which may be due to a small sample size. Training in neonatal resuscitation for midwives, nurses, pediatric residents, and obs-gyn residents should be emphasized.
Funding:The study was granted by the Of fi ce of Vice President for Research and Community Services of the University of Gondar.
Ethical approval:This study was approved by the institutional ethical review board of the University of Gondar, Gondar, Ethiopia.
Conflicts of interest:The authors do not have any conflict of interest.
Contributors:Gebreegziabher E conceived the study, developed the proposal, collected the data, analyzed the data and wrote the draft. Aregawi A and Getinet H were also involved in the proposal development, data collection, data analysis, paper writing, and manuscript preparation.
REFERENCES
1 Darmstadt GL, Lawn JE, Costello A. Advancing the state of the world's newborns. Bull World Health Organ 2003; 81: 224–225. Epub 2003 May 16.
2 Lawn EJ, Cousens S, Zupan J. For the Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: When? Where? Why? Lancet 2005; 365: 891–900.
3 Stein CE, Birmingham M, Kurian M, Duclos P, Strebel P. The global burden of measles in the year 2000-a model that uses country-specific indicators. J Infect Dis 2003; 187 Suppl 1: S8–14.
4 Lawn EJ, Osrin D, Adler A, Cousens S. Four million neonatal deaths: counting and attribution of cause of death. Paediatr Perinat Epidemiol 2008; 22: 410–416.
5 WHO Guidelines Approved by the Guidelines Review Committee. Guidelines on Basic Newborn Resuscitation. Geneva: World Health Organization; 2012.
6 Chiabi A, Nguefack S, Mah E, Nodem S, Mbuagbaw L, Mbonda E, et al. Risk factors for birth asphyxia in an urban health facility in cameroon. Iran J Child Neurol 2013; 7: 46–54.
7 Black ER, Cousens S, Johnson LH, Lawn EJ, Rudan I, Bassani GD, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010; 375: 1969–1987.
8 Bryce J, Boschi-Pinto C, Shibuya K, Black ER, the WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet 2005; 365: 1147–1152.
9 Mmbaga TB, Lie TR, Olomi R, Mahande JM, Kvåle G, Daltveit KA. Cause-specific neonatal mortality in a neonatal care unit in Northern Tanzania: a registry based cohort study. BMC Pediatrics 2012; 12: 116.
10 Levels & Trends in child mortality: Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. Report 2012.
11 Ogunlesi T, Adekanmbi F, Olanrewaju D, Olowu A. Comparative analyses of childhood deaths in Sagamu, Nigeria: implications for the fourth MDG. SAJCH 2007; 1: 106–111.
12 Kumbani CL, Sundby J, Odland OJ. Factors associated with perinatal deaths in women delivering in a health facility in Malawi. J Nurs Midwifery Res 2012; 1: 69–79.
13 Ibekwe PC, Ugboma HU, Oniyre N, Muokone U. Perinatal mortality in Southern Nigeria; less than half a decade to the millennium development goals. Ann Med Health Sci Res 2011; 1: 215–222.
14 Engmann C, Walega P, Aborigo RA, Adongo P, Moyer CA, Lavasani L, et al. Stillbirths and early neonatal mortality in rural Northern Ghana. Trop Med Int Health 2012; 17: 272–282.
15 Murila F, Obimbo MM, Musoke R. Assessment of knowledge on neonatal resuscitation amongst health care providers in Kenya. Pan Afr Med J 2012; 11: 78.
16 Ogunlesi AT, Dedeke IO, Adekanmbi AF, Fetuga MB, Okeniyi JA. Neonatal resuscitation: knowledge and practice of nurses in western Nigeria. SAJCH 2008; 2: 23–25.
17 Enweronu-Laryea C, Engmann C, Osafo A, Bose C. Evaluating the effectiveness of a strategy for teaching neonatal resuscitation in West Africa. Resuscitation 2009; 80: 1308–1311.
18 Kim MY, Ansari N, Kols A, Tappis H, Currie S, Zainullah P, et al. Assessing the capacity for newborn resuscitation and factors associated with provider's knowledge and skills: a cross sectional study in Afghanistan. BMC Pediatrics 2013; 13: 40.
19 Trevisanunuto D, Ibrahim AS, Doglioni N, Salvadoni S, Ferrarese P, Zanardo V. Neonatal resuscitation courses for pediatrics residents: comparison between Khartoum (Sudan) and Padowa (Italy). Paediatr Anaesth 2007; 17: 28–31.
20 Taksande MA, Vilhekar KY. Neonatal resuscitation training programme, its efficiency at rural hospital. Medical Journal of Islamic World Academy of Sciences 2012; 20: 6–9.
21 Jabir MM, Doglioni N, Fadhil T, Zanardo V, Trevisanuto D. Knowledge and practical performance gained by Iraqi residents after participation to a neonatal resuscitation program course. Acta Paediatrica 2009; 98: 1265–1268.
Received February 22, 2014
Accepted after revision June 15, 2014
World J Emerg Med 2014;5(3):196–202
10.5847/ wjem.j.issn.1920–8642.2014.03.007



